Abstract
Background and Objective: Melasma and acquired dermal
melanocytosis (ADM; acquired bilateral nevus of Ota-like
macules) are both symmetrically seen most commonly on
the face of women with darker skin, and are also known
as difficult conditions to treat.
Methods: Our topical bleaching protocol with 0.1-0.4%
tretinoin gel and 5% hydroquinone was repeatedly (1-3
times) performed for melasma (n=163), and a combination
treatment with the topical bleaching and Q-switched
ruby (QSR) laser was repeatedly (1-3 times) performed
for ADM (n=62).
Results: There is a significant correlation between
clinical results (clearance of pigmentation) and the
number of sessions in both melasma (P=0.019) and ADM
(P<0.0001).
Conclusion: The repeated treatment protocols for melasma
and ADM showed successful clinical results compared
to conventional ones, and they may be applied to other
pigmented conditions. It may be better that epidermal
and dermal pigmentations are treated separately, especially
in dark-skinned peoples who are more likely to suffer
post-inflammatory hyperpigmentation after inflammation-inducing
therapies.
Introduction
Melasma is acquired and symmetrical hypermelanosis,
usually widely spread on the malar prominence and cheek,
and less frequently on forehead and upper lip. Melasma
appears usually in the thirties or forties after pregnancy
or contraceptive use, suggesting that the triggering
of melasma is hormonal related1. Conventional treatments
for melasma include a sunscreen, hypopigmenting agents,
often in combination with other therapies, such as tretinoin,
topical corticosteroids, or superficial peeling agents2-7.
On the other hand, acquired dermal melanocytosis (ADM)
is a pigmented lesion involving bilateral grayish-brown
facial macules that was first reported as acquired bilateral
nevus of Ota-like macules (Hori’s nevus) by Hori et
al.8. ADM onsets usually in the twenties, represents
bilateral involvements, with the malar regions almost
always affected while the lateral forehead and nasal
alars are sometimes involved. The distribution pattern,
its grayish round-spot appearance with unclear margins,
and difference in color, are critical points to distinguish
with melasma. Since both melasma and ADM are bilateral
lesions and some patients have both, inexperienced doctors
could misdiagnose them.
Melasma and ADM are frequently seen in Oriental females,
and indeed 225 of 1,184 patients (19.1 %) who treated
pigmented skin problems in our outpatient clinic had
either or both. The authors previously described an
aggressive and optimal use of tretinoin along with hydroquinone
for various kinds of skin hyperpigmentation9-11 and
a combination therapy with Q-switched ruby (QSR) laser
for ADM12. The topical bleaching treatment with tretinoin
and hydroquine is a most effective tool for removal
of epidermal pigmentation. In this study, the clinical
results of repeated therapies for melasma and ADM was
analysed; we performed repeated tretinoin-hydroquinone
bleaching therapy for melasma, and a repeated combination
therapy of the topical bleaching and QSR laser for ADM.
Patients and Methods
Preparation of Ointments: Tretinoin aqueous gels (tretinoin
gel) at 3 different concentrations (0.1, 0.2, and 0.4
%) were originally prepared at the Department of Pharmacy,
University of Tokyo Hospital. The precise regimen of
tretinoin aqueous gel was described before10. These
gels can be prepared relatively easily, because the
tretinoin powder (Sigma Chemical, St. Louis, MO) is
commercially available. Aqueous gel is most suitable
for ointment base of tretinoin because of its good permeability.
An ointment including 5% hydroquinone and 7% lactic
acid (HQ-LA ointment), and one including 5% hydroquinone
and 7% ascorbic acid (HQ-AA ointment) were also prepared.
Plastibase? (petrolatum polyethylene ointment base,
Taisho Pharmacology, Osaka, Japan) was used as the ointment
base of the HQ-LA ointment, while hydrophilic ointment
was used for the HQ-AA ointment. Because tretinoin gel,
HQ-LA, and HQ-AA ointments (especially tretinoin gel)
are pharmacologically unstable, fresh ointments were
prepared at least once a month and stored in a dark
and cool (4oC) place.
Evaluations of results: Photographs were taken for every
patient at baseline and after treatment with a high-resolution
digital camera (Canon EOS-D30). The percentage of pigmentary
clearance was evaluated via the photographs by two experienced
plastic surgeons who did not perform this treatment.
The mean data of the pigmentary clearance of each patient
were classified into 4 categories: “excellent” (80%
or more clearance), “good” (50% to less than 80% clearance),
“fair” (0% to less than 50% clearance), and “poor” (no
change or worse).
Patients: Of 1,184 Asian patients who underwent cosmetic
treatments, 163 had melasma and 62 suffered from ADM
(6 had also melasma). All patients with melasma or ADM
were women except for 2 men with melasma. Patient age
at the start of the treatment of melasma and ADM patients
ranged from 27 to 62 years (42.3 ±7.1; mean ± S.D.)
and from 22 to 53 years (36.4 ±8.1), respectively.
Treatment Methods: For melasma, our topical bleaching
treatment (see below) was performed. If patients wanted,
the treatment was repeated two or three times. For ADM,
a combination therapy of the topical bleaching and QSR
laser was performed. The number of treatment sessions
depends on patient’s decision. Typical time courses
of the treatment protocols are shown in Fig.1a and 1b.
1) Topical bleaching treatment: The purpose of this
treatment is to improve epidermal pigmentation by accelerating
discharge of epidermal melanin (with tretinoin) and
suppressing new epidermal melanogenesis (with hydroquinone).
The two-staged (bleaching and healing) treatment was
performed as following:
a) Bleaching phase: 0.1 % tretinoin gel and HQ-LA ointment
were initially applied to the skin lesions twice a day.
Tretinoin gel was carefully applied only on pigmented
spots using a small cotton-tip applicator, while the
HQ-LA ointment was widely applied with fingers (e.g.
all over the face) a few minutes later, after allowing
the applied tretinoin aqueous gel get to dry. The method
of ointment application is critical in this aggressive
treatment in order to obtain maximal bleaching effects
with minimal irritant dermatitis. In cases in which
severe irritant dermatitis was induced by HQ-LA ointment,
HQ-AA ointment was used instead. Patients were requested
to visit our hospital at 1, 2, 4, 6 and 8 weeks after
starting this treatment, and every 4 weeks thereafter.
When the appropriate skin reaction (that is, mild erythema
and scaling) was not observed at 1 week, the concentration
of tretinoin was increased to 0.4 %, because 0.2% tretinoin
gel was usually not strong enough to get a sufficient
reaction in these cases. The concentration of tretinoin
and frequency of its application were appropriately
modified according to the skin condition and degree
of erythema and scaling. It took 4 to 8 weeks to finish
this phase. In the second or third bleaching treatment,
tretinoin gel of the final strength used in the first
step was used from the beginning.
b) Healing phase: After a 4-8 week bleaching phase,
the application of tretinoin gel and HQ-LA ointment
was discontinued, and application of HQ-AA ointment
was started in order to prevent post-inflammatory hyperpigmentation
(PIH) until the redness was sufficiently reduced. It
usually took 4 weeks to complete this phase. Topical
corticosteroids were not employed in either the bleaching
or healing phase.
2) QSR laser treatment: In patients with ADM, topical
anesthesia (lidocaine patch; PenlesR, Wyeth Lederle
Japan Inc., Tokyo, Japan) was applied 60-120 minutes
before the laser treatment. For QSR 694.5 nm laser (Model
IB101, Niic Co. LTD, Tokyo, Japan) treatment, spot size
of 5 mm, 1 Hz repeat rate, pulse duration of 20 ns,
and fluences ranged from 4.0 to 5.0 J/m2 were used.
After laser treatment, topical gentamicin sulfate ointment
(GentacinR, Schering-Plough, NJ) was applied twice a
day until a scale or thin crust disappeared (usually
5-7 days). At 2 weeks after laser treatment, application
of HQ-AA ointment was started.
At 4 weeks after each laser treatment, topical bleaching
treatment with tretinoin gel of appropriate concentration
(usually the same as the final concentration in the
bleaching phase) and HQ-AA ointment were started as
a pretreatment of the next laser irradiation, and also
as a treatment of post-laser PIH in some cases. In most
cases, a bleaching phase for 2 weeks was sufficient,
and we can usually estimate the clinical result at 8
weeks after each laser treatment. When some hyperpigmentation
remained, we can do another session.
Statistics: Spearman’s correlation coefficient by rank
test was used for analyzing a statistical significance
between the extent of clinical improvements and the
number of treatments.
Results
In 163 patients with melasma, 96 underwent only one
topical bleaching treatment (See Fig.1a) with excellent
results in 25 and good in 40; 56 underwent two treatments
with excellent results in 21 and good in 20; 11 underwent
three treatments with excellent results in 7 and good
in 3 (Table 1). In 62 patients with ADM, 16 underwent
only one treatment (a combination of topical bleaching
and QSR laser; See Fig.1b) with excellent results in
1 and good in 6; 26 underwent two treatments with excellent
results in 14 and good in 8; and 20 underwent three
treatments with excellent results in 17 and good in
3 (Table 2).
Representative cases with melasma are shown in Figs.
2 and 3, and those with ADM in Figs. 4 and 5.
Statistical analysis showed there is a significant correlation
between clinical results (clearance of pigmentation)
and the number of sessions in both melasma (P=0.019)
and ADM (P<0.0001). Discussion
The authors previously reported on a topical bleaching
therapy with aggressive use of retinoids in aqueous
gel only on the pigmented spot and use of hydroquinone
all over the face12,13. The treatment can clear only
epidermal pigmentation, but with excellent efficiency
compared to other conventional treatments such as
AHA peeling or single use of tretinoin or hydroquinone.
Corticosteroids are not used in the bleaching protocol,
and, furthermore, tretinoin is not continually used
over 2 months. It is well known that long term continual
use of tretinoin, either topical or oral, reduces
clinical effects of tretinoin14,15. It has been suggested
that this phenomenon may be due to intracellular production
of cellular retinoic acid binding proteins (CRABPs)
which is induced by the retinoid signal. This is why
we use repeated bleaching protocols with intervals
instead of continual use of tretinoin.
The present results demonstrated that the results
for ADM (excellent cases; excellent and good cases
= 6.3%; 43.8%) are not as good as for melasma (26.0%;
67.7%) in one-session cases, but in three-session
cases ADM was improved at a higher rate (85.0%; 100%)
compared to melasma (63.6%; 90.9%). Actually, we often
detected apparent improvement during the second session
in cases with ADM.
Melasma usually has most of its pigmentation in the
epidermis (Fig. 6). Although previous reports with
tretinoin, hydroquinone, AHA or others, or combinations
of multiple agents, showed moderate to relatively
good clearance of melasma2-7, complete clearance of
pigmentation is rare. Based on our experiences, the
differential uses of tretinoin and hydroquinone are
quite important for melasma, because if we use tretinoin
on a larger area such as the whole face, the surrounding
non-pigmented area is also bleached, and consequently,
the macules would remain clinically recognizable.
Although melasma is well-known as a hard condition
to treat, repetition of the topical bleaching only
on the pigmented area improved it completely in some
cases.
ADM has significant epidermal pigmentation, unlike
nevus of Ota, (Fig.6) and the fact suggests that clearance
of epidermal pigmentation before QSR treatment is
important in order to promote the efficiency of QSR
laser for dermal melanocytosis and to reduce PIH induced
by inflammation around the basal layer12. Topical
bleaching treatment clears post-inflammatory hyperpigmentation
induced by the QSR laser and also plays an important
role as a pretreatment for the next QSR irradiation.
The bleaching pretreatment for QSR laser therapy can
be applied to any other skin conditions with both
epidermal and dermal pigmentation, such as friction
melanosis and pigmented contact (cosmetic) dermatitis.
One typical case with pigmented contact dermatitis
is shown in Fig. 7 as a reference supplement. Compared
to lesions with dermal melanocytosis, those with dermal
melanosis were frequently treated with fewer QSR sessions.
Melasma and ADM are sometimes hard to distinguish
each other because they are both symmetrical, and
they coexist in some cases. Indeed, we have a few
cases in our series which were first diagnosed as
melasma, but dermal pigmentation was found after the
first topical bleaching and the diagnosis was corrected
to ADM later. In our repeated protocols the topical
bleaching treatment can be started in either condition,
so that the treatment plan can be corrected without
any loss of treatment periods.
We here proposed repeated treatment protocols for
melasma and ADM with successful effectiveness compared
to conventional ones, and they may be applied to other
pigmented conditions. It may be better that epidermal
and dermal pigmentations are treated separately, especially
in dark-skinned people who are more likely to suffer
PIH after inflammation-inducing therapies.
Figure Legends
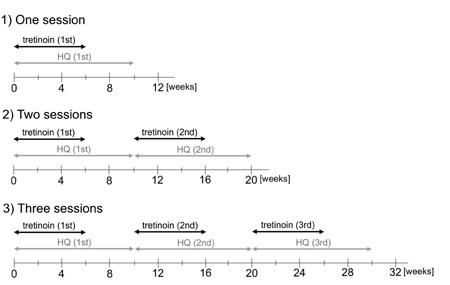
Fig. 1. (a) A representative time course of our topical
bleaching treatment with tretinoin and hydroquinone.
Tretinoin is used for 6 weeks in each bleaching phase,
and can be restarted with an at least 4 weeks interval
of healing phase.
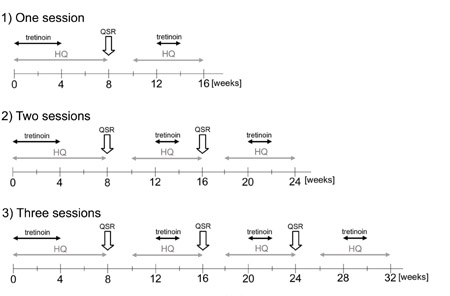
(b) A representative time course of the combined treatment.
Tretinoin is used for 4 weeks in the initial bleaching
pretreatment, and for 2 weeks in the following pretreatments.
If QSR laser treatment is performed 3 times, and the
total treatment period is 32 weeks.
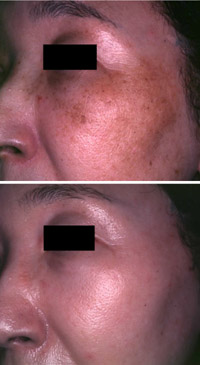
Fig. 2. Case1. (top) Baseline photo of a 47-year-old
woman with melasma. (bottom) At 5 months, the pigmentation
was cleared up after 3 sessions of topical bleaching
treatments.

Fig. 3. Case2. (top, left & right) A baseline
view of a 27-year-old woman with melasma. (bottom,
left & right) At 5 months, after 2 sessions of
QSR laser and topical treatments. The clinical result
was evaluated as “excellent”.

Fig. 4. Case3. (top) A baseline view of a 41-year-old
woman with ADM. (bottom) Two months after the 3rd
QSR laser treatment (8 months from the baseline).
The result of the clearance was evaluated as “excellent”.
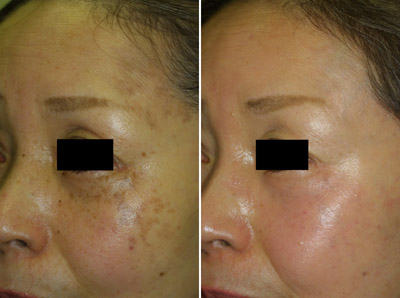
Fig. 5. Case 4. (left) A baseline view of a 49-year-old
woman with ADM. She had spotty pigmentations on the
cheeks, lateral foreheads, and nasal alars. (right)
After 3 sessions of QSR laser and topical treatments
(32 weeks from the baseline). The pigmentations were
almost completely cleared and also the yellowish color
of surrounding skin has changed to pinkish.
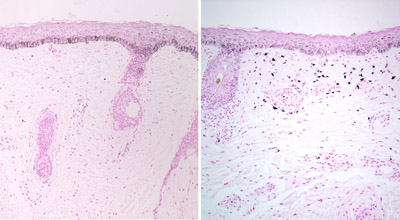
Fig. 6. Histology of melasma (left) and ADM (right)
before treatment. Melasma demonstrated epidermal hyperpigmentation
around the basal layer and very few in the dermis,
while ADM showed melanocytosis in the upper dermis,
as well as hyperpigmentation of the basal layer. (Masson-Fontana
staining; 100X)

Fig. 7. Case 5. This is not a case included in the
present study and only shown as a supplement for reference.
(left) Histology of pigmented contact (cosmetic) dermatitis
before treatment. The basement membrane is broken
down and a number of melanosomes were dropped into
the dermis (melanin incontinence). (Masson-Fontana
staining; 200X) (middle) At baseline, the patient
showed dark brown to dark grey macules distributed
symmetrically on a wide area of the face. The combined
therapy of QSR laser and topical bleaching was performed.
(right) At 4 months (one session of QSR laser treatment
with pre- and post-treatment of topical bleaching),
the pigmentation topical bleaching pretreatment. The
pigmentations were significantly improved by only
one session of the combined treatment. It may be that
dermal melanosis is easier to treat by laser than
dermal melanocytosis.
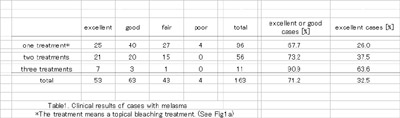
Table1. Clinical results of cases with melasma.
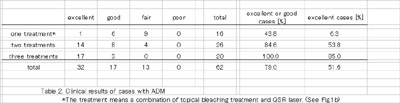
Table 2. Clinical results of cases with ADM.
References
1. Grimes PE. Melasma. Etiologic
and therapeutic considerations. Arch Dermatol 1995;131,1453-7.
2. Hurley ME, Guevara IL, Gonzales M, Pandya AG. Efficacy
of glycolic acid peels in the treatment of melasma.
Arch Dermatol 2002;138.1578-82.
3. Griffiths CE, Finkel LJ, Ditre CM, Hamilton TA,
Ellis CN, Voorhees JJ. Topical tretinoin (retinoic
acid) improves melasma. A vehicle-controlled, clinical
trial. Br J Dermatol 1993;129:415-21.
4. Nanda S, Grover C, Reddy BS. Efficacy of hydroquinone
(2%) versus tretinoin (0.025%) as adjunct topical
agents for chemical peeling in patients of melasma.
Dermatol Surg 2004;30:385-8.
5. Sarkar R, Bhalla M, Kanwar AJ. A comparative study
of 20% azelaic acid cream monotherapy versus a sequential
therapy in the treatment of melasma in dark-skinned
patients. Dermatology 2002;205:249-54.
6. Lawrence N, Cox SE, Brody HJ. Treatment of melasma
with Jessner's solution versus glycolic acid: a comparison
of clinical efficacy and evaluation of the predictive
ability of Wood's light examination. J Am Acad Dermatol
1997;36:589-93.
7. Garcia A, Fulton JE Jr. The combination of glycolic
acid and hydroquinone or kojic acid for the treatment
of melasma and related conditions. Dermatol Surg 1996;22:443-7.
8. Hori Y, Kawashima M, Oohara K, Kukita A. Acquired,
bilateral nevus of Ota-like macules. J Am Acad Dermatol
1984;10:961-4.
9. Yoshimura K, Harii K, Aoyama T, et al. A new bleaching
protocol for hyperpigmented skin lesions with a high
concentration of all-trans retinoic acid aqueous gel.
Aesthetic Plast Surg 1999;23:285-91.
10. Yoshimura K, Harii K, Aoyama T, Iga T. Experience
with a strong bleaching treatment for skin hyperpigmentation
in Orientals. Plast Reconstr Surg 2000;105:1097-108.
11. Yoshimura K, Momosawa A, Watanabe A, et al. Cosmetic
color improvement of the nipple-areola complex by
optimal use of tretinoin and hydroquinone. Dermatol
Surg 2002;28:1153-8.
12. Momosawa A, Yoshimura K, Uchida G, et al. Combined
Therapy Using Q-Switched Ruby Laser and Bleaching
Treatment with Tretinoin and Hydroquinone for Acquired
Dermal Melanocytosis. Dermatol Surg 2003;29:1001-7.
13. Yoshimura K, Momosawa A, Aiba E, et al. Clinical
trial of bleaching treatment with 10 % all-trans retinol
gel. Dermatol Surg 2003;29:155-60.
14. Muindi J, Frankel SR, Miller WH Jr, et al. Continuous
treatment with all-trans retinoic acid causes a progressive
reduction in plasma drug concentrations: implications
for relapse and retinoid "resistance" in
patients with acute promyelocytic leukemia. Blood.
1992;79:299-303.
15. Regazzi MB, Iacona I, Gervasutti C, Lazzarino
M, Toma S. Clinical pharmacokinetics of tretinoin.
Clin Pharmacokinet 1997;32:382-402. |