Abstract
Background: A prominent mandibular angle is a relatively
common aesthetic problem among Orientals, and reduction
angle-splitting ostectomy is now becoming a very popular
procedure in Asian countries. Although this operation
is usually performed on young patients, the same aesthetic
demands are also seen in the elderly.
Methods: In this report, we describe our experience
of angle-splitting ostectomy on five patients over 50
years old. The operation procedure was the same as performed
in young patients, and clinical results were assessed
with photos and 3D-CTs.
Results: The aesthetic results of the facial contours
were satisfactory, but patients usually showed postoperative
redundancy of the skin especially along the jaw line
because of the loss of bony protrusion laterally. Therefore,
3 of the 5 cases underwent subsequent SMAS cheek lift.
The inferior alveolar nerve was damaged in one case
partly due to an atrophied mandibular bone with loss
of molars and premolars, so more care should be taken
in elder patients.
Conclusions: Angle-splitting ostectomy can be safely
and effectively performed on the elderly when the surgeons
are aware of the risks and indications specific for
the elderly patients, and a multidisciplinary support
system is available.
Introduction
A prominent mandibular angle is a relatively common
aesthetic problem among Orientals, and reduction angle-splitting
ostectomy is now becoming a very popular procedure in
Asian countries1-3. As reported previously, most of
patients who undergo reduction mandibuloplasty are young,
and elderly patients are very rare.
It is of note that aesthetic problems related to a prominent
mandibular angle are twofold in the elderly. One is
the same as in younger patients: broadness of the lower
face with an angular contour gives a strong impression,
undesirable in most Asian females. This type of aesthetic
demand is seen in elderly as well as younger patients.
Another point is more specific to the elderly: rhytidectomy
in the elderly is generally less effective in Asian
patients with a prominent mandibular angle than in Caucasians.
Prominence of the mandible disturbs the smooth excursion
of lifting skin in the dissected cheek, and this problem
is frequently and specifically encountered in Asian
women4. In these contexts, reduction ostectomy of the
mandibular angle for the elderly is well justified,
although most previous publications mentioned only younger
cases.
In the past two years, we performed angle-splitting
ostectomy on five elderly Japanese patients over fifty
years old. Three of them had rhytidectomy afterwards
and one of the others is planning to. Some special considerations
should be required for managing these cases, and if
they are kept in mind, we believe that this operation
can be safely and effectively performed in elderly patients.
We herein describe our experiences in detail, and discuss
some features of this operation specific for the elderly
cases.
Materials and Methods
Patients
In the past two years, we performed angle-splitting
ostectomy on five Japanese patients over fifty years
old (Table 1). All of the patients had this operation
for a purely aesthetic purpose, and none had specific
craniofacial anomalies. Three of them had operation
of rhytidectomy several months later. None had simultaneous
ostectomy and rhitidectomy. We found no particular
risks for general anesthesia in these patients in
preoperative examinations, and all cases underwent
surgery under general anesthesia. We routinely suggested
patients to give 400 ml of their own blood at the
time of preoperative examinations for auto-transfusion,
and four of five patients did so.
Operative Procedures
The operations were performed mostly according to
previous publications by Deguchi et al.2 and Han and
Kim3, with slight modifications. In brief, the oral
mucosa was incised along the mandibular ramus, from
the point just beside the parotid papilla to the first
molar. The lateral surface of the mandibular angle
was exposed by subperiosteal dissection. The caudal
end of the masseter muscle was carefully released
from the mandible, but we did not cut or resect the
muscle berry. A deep groove was hollowed out on the
lateral cortex using a round burr, along the upper
and anterior boundary of the ostectomized area (Fig.
1A). Several perforations were made using a Lindemann
drill burr (Downs Surgical, Sheffield, UK) from this
groove toward the posterior and inferior margin of
the mandible, in parallel with and just under the
lateral cortex, to avoid any unexpected malfracture
(Fig. 1B). Then, the lateral cortex of the angular
bone was ostectomized with a bone chisel. If necessary,
the tip of the angle can be additionally excised with
an oscillating saw (Fig. 1C). The released end of
the masseter muscle was left detached. Finally, a
Penrose drain was inserted, the oral mucosa was closed
with absorbable 4-0 sutures, and a pressure mask was
applied and left overnight. The Penrose drains were
removed a few days later.
Results
The splitting-angle ostectomy was performed successfully
in all cases. Avarage operation time was 2 hours and
50 minutes. Average amount of hemorrhage was 500 ml,
and the four patients who gave their own blood preoperatively,
underwent auto-transfusion just before finishing surgery.
No patients required blood transfusions from other
persons. No malfractures of the mandible body, ramus
or condyle occurred. The right inferior alveolar nerve
was unexpectedly damaged during the splitting ostectomy
in one patient (Case 5). In this case, the ramus was
atrophic, possibly due to previous extraction of the
molars and premolars. The nerve was repaired with
8-0 nylon sutures and fibrin glue.
Postoperative recovery of general conditions was uneventful,
and no patients exhibited circulatory or respiratory
problems. No hematomas or no local infections were
observed. Transient unilateral sensory disturbance
of the skin in the mental nerve area was observed
in two cases (in addition to Case 5), and slight paralysis
of the marginal mandibular branch of the facial nerve
was seen for a few days in one case. Aesthetic outcomes
were quite satisfactory in all cases. Skeletal contours
of the lower face were significantly changed. Effects
of the facelift were remarkable in the three patients
who underwent subsequent rhytidectomy.
Case 1
A 55-year-old woman sought treatment for prominent
mandibular angle (Figs. 2A and 2D). She had a constant
complaint about the shape of her mandible from her
teenage. Also she wished to undergo a face-lift. She
had no special history of past illness. X-rays and
3D-CTs showed remarkable protrusion and lateral flaring
of the mandibular angle (Figs. 2G and 2I). The angle-splitting
ostectomy was performed under the general anesthesia,
and 5 x 2.5 cm fragments of the lateral cortex were
removed bilaterally. Postoperative X-rays and 3D-CTs
showed significant reduction of the lateral cortex
(Figs. 2H and 2J), and her facial contour was remarkably
changed two months after the ostectomy (Figs. 2B and
2E).
A rhytidectomy with radical SMAS lift was performed
three months after the ostectomy. The lifting was
very effective for reducing redundancy of the skin
in the mandibular area (Figs. 2C and 2F). No specific
problem was observed except slight and transient sensory
disturbance in her left lower lip. The patient was
very satisfied with the final result.
Case 2
A 65-year-old woman was referred to us for treatment
for her facial contour (Fig. 3A). She had been unhappy
with her angled face and low nose since childhood.
She had a history of asthma, but no attacks in the
last 10 years. A preoperative spirogram showed no
problems, and she underwent angle-splitting ostectomy
under general anesthesia. The angled contour was improved,
but the upper part of the angle was not completely
resected (Fig 3b). Seven months later, we performed
a correction of mandibular angle--through a facelift
incision with great care not to damage the submandibular
branch of the facial nerve-- together with an SMAS
facelift and insertion of silicone implants into her
nasal dorsum. The final result was very satisfactory
(Fig.3C).
Case 3
A 51-year-old housewife had a complaint about her
prominent zygoma and mandible (Figs. 4A and 4C). She
underwent a resection of the uterus myoma several
years ago, but had no other particular history. In
this case, the lateral flaring was not so remarkable,
but the whole mandibular angle was hypertrophic in
the preoperative 3D-CT (Fig. 4E). She underwent angle-splitting
ostectomy under general anesthesia. Postoperative
recovery was uneventful. A SMAS lift was performed
five months later, and the postoperative contour was
markedly improved (Figs. 4B, 4D and 4F).
Discussion
There have been a number of reports on surgical methods
for angular faces. This condition was historically
called "benign masseteric hypertrophy",
and resection of the masseter muscle as well as bone
was originally regarded as essential5,6. However,
angled appearance of the face in Orientals can be
primarily attributed to a lateral flaring of the bony
angle7. The masseter muscle, which always exhibits
tetanic contration, as do the calf muscles, can be
atrophied only by releasing the end of the muscle3,
and also by inducing temporal paralysis with Botulinus
toxin8. Therefore, the mandibular angle ostectomy
without muscle reduction can be a primary procedure
sufficient for this condition. Some authors reported
a simple full-thickness excision of the protruding
part of the bony angle1,7,9, which may often be accompanied
by an unnecessary change of SN/MP angle. Therefore,
a lateral cortical reduction by angle-splitting ostectomy
is now the first choice of operative options for the
majority of patients2,3.
In this paper, we described our experience of the
angle-spliting ostectomy in five aged Japanese women.
Most of the operative procedures are the same as in
younger patients, and the aesthetic results were quite
satisfactory. The final results were most dramatic
when the ostectomy was combined with subsequent rhytidectomy,
as seen in Cases 1, 2 and 3. It has been pointed out
that rhytidectomy in Asians requires special considerations,
because the facial skeletal contour in Orientals is
round and squared as Shirakabe et al. described in
the "baby model" paradigm4,10. Oriental
skin is thicker than that of Caucasians with abundant
extracellular matrices10, and this fact also contributes
to the difficulty of Asian rhytidectomy. In this sense,
after correcting angular skeletal contours with angle-splitting
ostectomy, facelift can be performed more easily in
Orientals with ideal clinical results. Baek et al.7
also reported a combination of angle ostectomy and
rhytidectomy in several patients, the two procedures
performed simultaneously in their cases. However,
we prefer two-stage operations with an interval of
several months for the following reasons. One reason
is to avoid lengthy operation time, considering that
Orientals need vigorous SMAS lift as noted above.
Delicate adjustment of the bony angle shape can be
achieved in the second operation through a facelift
incision as seen in Case 2--another advantage of our
two-stage strategy. We consider the most important
reason to be that sufficient lifting is likely impossible
in the one stage operation due to intraoperative swelling
caused by the ostectomy.
Several problems should be borne in mind when the
angle-splitting ostectomy is performed on the elderly.
Most important is atrophy of the mandible, as seen
in Case 5. In this case, the inferior alveolar nerve
was damaged during the splitting ostectomy partly
due to the thinness of the bony angle. As stated by
Moss and Salentijn11 in their "functional matrix"
concept, craniofacial bone remodeling is mainly controlled
by external mechanical stresses. The edentulous mandible
in the elderly often exhibits remarkable atrophy mainly
in the alveolus by the loss of stress through the
teeth12. In Case 5, the bilateral molars and premolars
were missing and the 3D-CT revealed atrophy and thinness
around the mandibular angle (Figs. 5A and 5B). However,
we can also detect in this CT a remarkable lateral
flaring of the angle, which causes a prominent mandibular
angle (Figs. 5B and 5C). The mechanisms by which the
functional matrix works are completely different between
the alveolus and the lateral flaring of the angle,
because the bone deposition in the lateral cortex
of the mandibular angle is considered to be affected
by the tention of the masseter muscle13. This is the
reason why a prominent mandibular angle can be observed
even in the edentulous atrophic mandible. We can treat
such cases with reduction mandibuloplasty, but special
care should be taken not to damage the inferior alveolar
nerve and to avoid malfractures. It is reported that
the mandibular canal remains intact around the angle
even in the completely edentulous mandible12, and
this fact supports our opinion that angle-splitting
can be safely performed if the surgeons are well acquainted
with the specific features of mandibular atrophy in
elderly patients. Preoperative 3D-CTs may be quite
informative for this purpose.
Other risks of the angle-splitting ostectomy include
hemorrhage from branches of the facial artery. We
encountered a relatively large amount of hemorrhage
in three patients. This risk can be minimized by preparation
of the auto-blood transfusion. Collaboration with
anesthesiologists is also essential for avoiding general
risks potentially serious in the elderly, and with
their help we did not experience any circulatory or
respiratory troubles pre- or post-operatively.
In conclusion, we believe the angle-splitting ostectomy
for the prominent mandibular angles can be safely
and effectively performed on elderly patients, if
the surgeon is well acquainted with the specific features
in elderly cases, and a multi-disciplinary support
system is available.
Legends
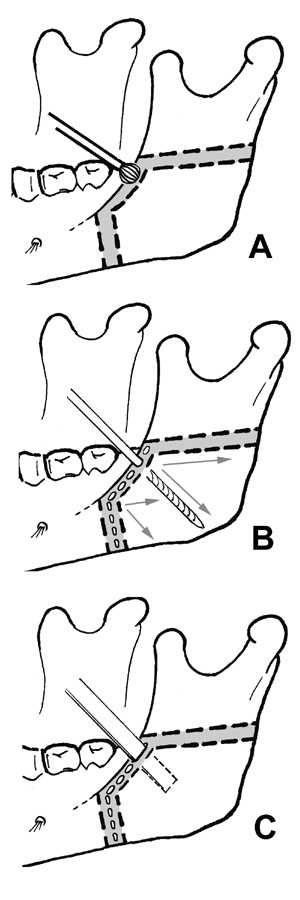
Fig.1 Illustrations of the operative procedures. (A)
A deep groove is made along the shaded area (upper
and anterior boundary of the ostectomy), using a round
burr. (B) Several perforations are made using a Lindemann
drill burr from this groove in various directions
(arrows). (C) The lateral cortex of the angular bone
is ostectomized with a bone chisel. The tip of the
angle is additionally excised with an oscillating
saw, if necessary.
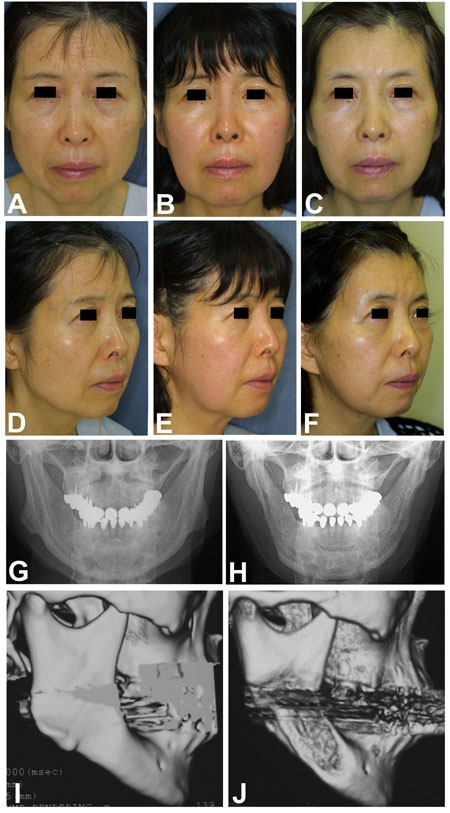
Fig.2 Case 1. A 55-year-old woman. (A, D) Preoperative
appearance. (B, E) Two months after the ostectomy.
(C, F) Two months after the SMAS lift. (G) Preoperative
frontal cephalogram shows remarkable lateral flaring
of the mandibular angle. (H) Post-ostectomy cepharogram.
(I) Preoperative 3D-CT. (J) Post-ostectomy 3D-CT reveals
a successful reduction of the angle.
 Fig.3
Case 2. A 65-year-old woman. (A) Preoperative appearance.
(B) Appearance after the angle-splitting ostectomy.
Some protrusion is left in the angle. (C) Final appearance,
1 year after the ostectomy and five months after the
SMAS lift. The angle shape was adjusted through the
facelift incision. She also underwent augmentation
of the nose at the secondary operation. Fig.3
Case 2. A 65-year-old woman. (A) Preoperative appearance.
(B) Appearance after the angle-splitting ostectomy.
Some protrusion is left in the angle. (C) Final appearance,
1 year after the ostectomy and five months after the
SMAS lift. The angle shape was adjusted through the
facelift incision. She also underwent augmentation
of the nose at the secondary operation.
Fig.4 Case 3. A 51-year-old woman.
(A,C) Preoeprative appearance. (B, D) Postoperative
appearance, 8 months after the ostectomy and three
months after the SMAS lift. (E) Preoperative 3D-CT
reveals remarkably hypertrophic angle of the mandible.
(F) Postoperative 3D-CT shows that the ostectomy was
effective.
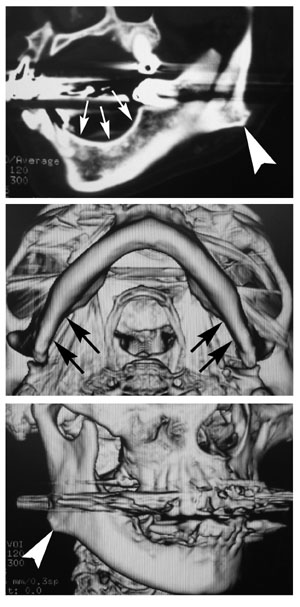 Fig.5
Preoperative CT of the edentulous mandible of Case
5, a 69-year-old woman. (A) CT of the oblique plane
of the left mandibular angle. Note the lateral flaring
of the angle (arrowhead) even though the mandibular
body shows remarkable atrophy (arrows) due to the
extraction of the molars and premolars. (B) A caudal
view of the mandible by 3D-CT shows atrophy around
the angle (arrows). (C) A lateral view of the mandibular
angle by 3D-CT. The lateral flaring is obviously noted
(arrowhead). Fig.5
Preoperative CT of the edentulous mandible of Case
5, a 69-year-old woman. (A) CT of the oblique plane
of the left mandibular angle. Note the lateral flaring
of the angle (arrowhead) even though the mandibular
body shows remarkable atrophy (arrows) due to the
extraction of the molars and premolars. (B) A caudal
view of the mandible by 3D-CT shows atrophy around
the angle (arrows). (C) A lateral view of the mandibular
angle by 3D-CT. The lateral flaring is obviously noted
(arrowhead).
Table 1. Patient Profiles
Case
number age sex operation time bleeding (ml) auto-blood
transfusion intraoperative
nerve injury subsequent
face lift follow
-up
1 55 F 2h25m 400 + - + 1y11m
2 65 F 1h55m 100 - - + 1y2m
3 51 F 2h15m 560 + - + 8m
4 61 F 3h00m 670 + - - 6m
5 69 F 4h20m 770 + + - 3m
References
1. Baek, S. M., Kim, S. S., and Bindiger,
A. The prominent mandibular angle: preoperative management,
operative technique, and results in 42 patients. Plast
Reconstr Surg 83: 272, 1989.
2. Deguchi, M., Iio, Y., Kobayashi, K., and Shirakabe,
T. Angle-splitting ostectomy for reducing the width
of the lower face. Plast Reconstr Surg 99: 1831, 1997.
3. Han, K., and Kim, J. Reduction mandibuloplasty:
ostectomy of the lateral cortex around the mandibular
angle. J Craniofac Surg 12: 314, 2001.
4. Shirakabe, Y. The Oriental aging face: an evaluation
of a decade of experience with the triangular SMAS
flap technique in facelifting. Aesthetic Plast Surg
12: 25, 1988.
5. Adams, W. Bilateral hypertrophy of the masseter
muscle: An operation for correction (case report).
Br J Plast Surg 2: 78, 1949.
6. Ousterhout, D. K. (1991). "Mandibular width
reduction including the surgical treatment of benign
masseteric hypertrophy." Aesthetic contouring
of the craniofacial skeleton, D. K. Ousterhout, ed.,
Little, Brown, Boston, 451.
7. Baek, S. M., Baek, R. M., and Shin, M. S. Refinement
in aesthetic contouring of the prominent mandibular
angle. Aesthetic Plast Surg 18: 283, 1994.
8. Lindern , J.J., Niederhagen, B., Appel, T., Berge,
S., Reich, R.H. Type A botulinum toxin for the treatment
of hypertrophy of the masseter and temporal muscles:
an alternative treatment. Plast Reconstr Surg 107:327,
2001.
9. Yang, D. B., and Park, C. G. Mandibular contouring
surgery for purely aesthetic reasons. Aesthetic Plast
Surg 15: 53, 1991.
10. Shirakabe, Y., Suzuki, Y., and Lam, S. M. A new
paradigm for the aging Asian face. Aesthetic Plast
Surg2003.
11. Moss, M. L., and Salentijn, L. The primary role
of functional matrices in facial growth. Am J Orthod
55: 566, 1969.
12. Polland, K. E., Munro, S., Reford, G., et al.
The mandibular canal of the edentulous jaw. Clin Anat
14: 445, 2001.
13. Cutting, C. B., McCarthy, J., G., and Knoze, D.
M. (1990). "Repair and Grafting of Bone."
Plastic Surgery Vol.1, J. G. McCarthy, ed., W.B.Saunders
Company, Philadelphia, 583.
|