|
Abstract
Background: A successful treatment to improve the color of
nipple-areola complex (NAC) has never been reported,
although the number of women seeking the more attractively
colored NAC is not small.
Objective: To determine the effectiveness of our bleaching
protocol for cosmetic improvement of NAC.
Methods: The protocol was composed of two phases: bleaching
phase (4-8 weeks) and healing phase (2-6 weeks). 0.2-0.4%
tretinoin aqueous gel was applied concomitantly with 5% hydroquinone,
7% lactic acid ointment for bleaching twice a day. Tretinoin
was applied on NAC with a small cotton applicator, while
hydroquinone was widely applied beyond the NAC area. After
obtaining sufficient improvement in NAC color, the application
of tretinoin was discontinued and hydroquinone alone was
continually applied in the healing phase until the reactive
erythema was eliminated. Fifteen female patients were involved
in this study.
Results: The average treatment period was 16.6 weeks. Improvement
of NAC color was obtained in 12 patients (80 %) by the physicians'
estimation, and 11 patients (73 %) satisfied with their final
results. The treatment was repeated after a 1-month interval
of tretinoin application in 4 patients: 2 desired further
improvement in color, and 2 had the second course conducted
to treat the postinflammatory hyperpigmentation on the surrounding
mound induced by the first course.
Conclusion: The treatment appeared to be most effective for
cosmetic improvement of NAC color among treatments available
so far.
Introduction
The number of females seeking a better-looking nipple-areola
complex (NAC) is not small. Some patients complain about
the size of nipple and/or areola, and others about the color
of NAC; the number of the latter is apparently greater in
Japan. In general, patients prefer lighter color to darker
color. An NAC which looks bright pink is thought to be more
attractive than a dark-brown one. Some patients have dark-looking
NAC from childhood, but others develop them in adolescence
or later. Upregulations of female hormones after adolescence
could affect the color of the NAC, and repeated mechanical
stimulations such as rubbing by undergarments or sexual habits
??? can leave postinflammatory hyperpigmentation on NAC.
No satisfactory method has ever been reported for treatment
of NAC color, although there are several options: laser therapies,
chemical peeling and tattooing. Lasers, such as Q-switch
ruby laser, Q-switch Nd:YAG laser, and dye lasers, can change
the color, but the results are often disappointing and can
be miserable. Laser treatments for NACs sometimes lead to
depigmentation and/or scarring, and it is hard to get a homogenous
and natural appearance. Chemical peeling such as alpha-hydroxy
acids or TCA combined with a bleacher such as hydroquinone
is minimally effective in changing NAC color. Tattooing with
white or pink color leads to unnatural appearance, recovery
from which is almost impossible.
The authors previously described an aggressive and optimal
use of tretinoin along with hydroquinone for various kinds
of skin hyperpigmentation [1, 2]. More than 8,000 patients
with hyperpigmented skin lesions have been treated with the
original method or its modifications in our facility over
the past 7 years with successful overall results. In the
present study, the modified protocol was applied to the patients
who wanted improved NAC color, and the results were satisfactory.
To our knowledge, this paper is the first one to demonstrate
successful results on NAC color.
Patients and Methods
Preparation of Ointments: Tretinoin aqueous gels (tretinoin
gel) at 2 different concentrations (0.2, and 0.4 %) were
originally prepared at the Department of Pharmacy, University
of Tokyo, Graduate School of Medicine. The precise regimen
of tretinoin aqueous gel was described before (2). An ointment
including 5% hydroquinone and 7% lactic acid (HQ-LA ointment),
an ointment including 5% hydroquinone and 7% ascorbic acid
(HQ-AA ointment), and an ointment including 5% kojic acid
(KA ointment) were also prepared as well. Plastibase (petrolatum
polyethylene ointment base, Taisho Pharmacology, Osaka, Japan)
was used as the ointment base of the HQ-LA ointment, while
the hydrophilic ointment was used for the HQ-AA and the KA
ointments. Because tretinoin gel, HQ-LA, HQ-AA, and KA ointment
(especially tretinoin gel) are pharmacologically unstable,
fresh ointments were prepared at least once a month and stored
in a dark and cool (4oC) place.
Evaluations of results:
1) Clinical evaluations: Photographs were taken for every
patient at baseline and after the treatment, and two experienced
doctors (a dermatologist or cosmetic surgeon) who did not
perform this treatment evaluated the clinical results via
the photographs. The results were classified into 4 categories; "excellent" (improvement
is apparent and the result is impressive), "good" (improvement
can be recognized easily), "fair" (improvement
can be recognized anyhow), and "poor" (improvement
can not be recognized via photos).
2) Patient satisfaction: Patients were interviewed about
their level of satisfaction with the clinical results after
the treatment. The patient was requested to estimate the
clinical result and select one of three categories; "very
satisfied", "slightly satisfied", and "not
satisfied".
Patients: Each ointment was topically applied under signed
informed consent in 19 Japanese women with complaint about
their NAC color, and 15 of them who were followed up for
more than 12 weeks were analyzed in this study. The other
4 patients could not be followed up for more than 12 weeks,
and some of them might discontinue the treatment because
of irritation, although the reasons for them remain unclear.
The age of patients varied from 18 to 42 years old (age=32.1±4.2;
mean S.D.).
Treatment protocol: Our bleaching protocol is composed of
two phases, a bleaching phase and a healing phase. In the
bleaching phase, the pigmentation is aggressively treated,
and transient adverse skin effects such as erythema and irritation
are usually observed. Once satisfactory improvement is obtained,
the healing phase is started in order to reduce the erythema
and inflammation, taking care not to induce new postinflammatory
hyperpigmentation.
1) bleaching phase: Tretinoin gel and HQ-LA ointment were
applied to the NAC twice a day. 0.2% tretinoin was used initially.
Tretinoin gel was applied only on NAC areas using a small
cotton-tip applicator, while HQ-LA ointment was applied beyond
the NAC area (e.g. all over the whole breast mound). In cases
in which severe irritant dermatitis was induced by HQ-LA
ointment, HQ-AA or KA ointment was used instead. Patients
were requested to visit our hospital at 1, 2, 4, 6 and 8
weeks after starting this treatment, and every 4 weeks afterwards.
When the appropriate skin reaction (that is, mild erythema
and scaling) was not observed at 1 week, the concentration
of tretinoin was changed to 0.4%. In most cases, it took
4 to 8 weeks to finish this phase. If the patients desire
further improvement, the second treatment course with the
same protocol can be started after 4-6 weeks' interval (=
healing phase described below) of tretinoin gel application.
2) healing phase: After sufficient improvement of NAC color
was obtained, the application of tretinoin gel was discontinued,
but that of HQ-LA ointment was continued. In cases in which
erythema was not reduced at all after a few weeks' application
of HQ-LA ointment, HQ-LA ointment was also discontinued and
HQ-AA or KA ointment was applied until the redness was sufficiently
reduced. It usually took 4-6 weeks to complete this phase.
The total period of a single treatment course to finish both
phases was usually 8-12 weeks. Topical corticosteroids were
not employed either in the bleaching or healing phase.
Results
In general, erythema was seen in a few days, followed by
continual scaling during the first week. Erythema and scaling
were usually continually seen throughout the bleaching phase.
Formation of scales (accumulated horny layers) and itching
were also seen in some cases during the second week. After
the scales repeatedly came off, improvement of NAC color
was usually obtained. Sufficient improvement in NAC color
was obtained after a bleaching phase of 4-8 weeks in most
cases. During the healing phase, erythema was gradually reduced,
while the improvement in NAC color was maintained.
The average treatment period of 15 patients was 16.6 weeks,
because some cases underwent the second course. The second
treatment course was performed in 4 cases: 2 desired further
improvement in color, and 2 were treated for postinflammatory
hyperpigmentation on the surrounding mound induced by the
first course.
Of 15 patients, HQ-AA ointment was alternatively used to
reduce irritant dermatitis in 2 and 4 cases during the bleaching
and the healing phase, respectively, while KA ointment was
used in one case during the healing phase. No allergic contact
dermatitis to hydroquinone was seen in this study.
The clinical results and the patients' satisfaction were
summarized in Table 1. Two patients were evaluated as "excellent",
7 cases as "good", and 3 cases as "fair".
No improvement was clinically observed in the other 3 cases.
Some improvement was seen in 12 of 15 patients (80.0%).
Six patients achieved sufficient satisfaction with the results,
and 5 had slight satisfaction. The other 4 cases were not
satisfied with their results. Some satisfaction was recognized
by 11 of 15 patients (73.3%).
The representative 4 cases are shown in Figs. 1-4.
Discussion
It is generally quite difficult to treat disfiguring color
of the NAC, so no satisfactory treatment has been reported
so far. Laser treatments such as Q-switch ruby laser frequently
result in depigmentation and/or scarring (Fig. 5). Based
on our experiences with an aggressive bleaching treatment
using tretinoin and hydroquinone on thousands of patients,
the authors applied the modified protocol to treat NAC color,
and found it was sufficiently effective. This protocol can
eliminate melanin pigmentation quite effectively, although
patients experience unpleasant irritant dermatitis, especially
in the first 2 weeks. Some of the adverse effects during
the bleaching phase can be somewhat suppressed by use of
antioxidant lotions, moisturizing lotions/creams, and/or
oils. Corticosteroid ointments should not be used in this
treatment, the reason for which is mentioned below.
Since Kligman and Willis [3] introduced their depigmenting
formula, a number of products based on it such as TriLuma
have become commercially available. Those products contain
tretinoin and hydroquinone along with corticosteroid, and
can let patients treat their pigmentation in a simple manner
without having severe irritation. However, we believe that
corticosteroid reduces not only irritant dermatitis but also
depigmenting effects of tretinoin by suppressing keratinocytes
proliferation and epidermal turnover. Indeed, based on our
initial experiences, a concomitant use of corticosteroid
with tretinoin reduced significantly the effectiveness of
this treatment. In addition, the separate preparation of
tretinoin and hydroquinone is important, because it enables
differential applications of the two agents with regards
to the applied area and application periods, which are essential
in our protocol. We think the critical points of this protocol
are: 1) to use a high concentration of tretinoin "aqueous
gel ", which means an aggressive and optimal use of
tretinoin, 2) to not use corticosteroid at all, 3) to use
tretinoin only on the hyperpigmented lesion with a small
cotton-tip applicator and use hydroquinone over the large
area, including the surrounding area, and 4) to use hydroquinone
for at least 4 more weeks after cessation of tretinoin application.
The 3rd and 4th points are quite important to avoid postinflammatory
hyperpigmentation. Strictly speaking, the optimal amount
of tretinoin to administer changes day by day with skin conditions:
condition of the stratum corneum, the state of tolerance
to tretinoin, and personal variances.
The biological roles of tretinoin and hydroquinone in this
treatment should be clearly understood. The authors think
that the role of tretinoin in this protocol is to wash the
melanin granules out of the epidermis [4]. Tretinoin can
directly accelerate epidermal turnover (promote differentiation
of keratinocytes) and indirectly promote the proliferation
of keratinocytes. The reason for epidermal hyperplasia after
tretinoin application had been unknown, but tretinoin was
recently found to promote proliferation of keratinocytes
by inducing heparin-binding EGF like growth factor (HB-EGF)
secretion from suprabasal keratinocytes [5-7]. These beneficial
effects induced by tretinoin are specific for retinoids;
can not be obtained by chemical peeling agents such as AHA
and TCA, and can be greatly suppressed by corticosteroids.
The anti-retinoid effects of corticosteroids seen in vivo
are partly explained by the down-regulation of keratinocyte
growth factor expression from dermal fibroblasts induced
by corticosteroids [8]. The reason why the pigmentation in
the upper dermis is also reduced by tretinoin application
remains to be elucidated.
The role of hydroquinone, on the other hand, is to strongly
suppress production of new melanin. This is quite important
in the present treatment because tretinoin appears not to
suppress the melanin production as shown in our previous
study using pigmented skin equivalents [4]. According to
our experiences, the effectiveness of hydroquinone is far
larger than that of kojic acid, which can not necessarily
prevent postinflammatory hyperpigmentation induced during
the bleaching phase. It is our understanding that application
of corticosteroids is not beneficial to avoid postinflammatory
hyperpigmentation.
Virtually the only possible complication seen in this study
was postinflammatory hyperpigmentation because of irritant
dermatitis induced by aggressive use of tretinoin and/or
hydroquinone. In our experience, it occurred on breasts more
frequently than on faces with the same treatment. Therefore,
it may be better to use tretinoin on the area 2-3 mm in from
the areola margin, and hydroquinone just on the exact area
of the areola. It can not be denied that pigment darkening
would occur if continual application of hydroquinone was
not conducted after treatment. Rubbing daily the tissue by
undergarments could induce repeated inflammation followed
by postinflammatory hyperpigmentation. Postinflammatory hyperpigmentation
could be treated in most cases with HQ-AA ointment in a few
months. Otherwise, mild and careful use of tretinoin with
hydroquinone can treat it in a shorter period.
Conclusions
In the present clinical trials, our protocol improved NAC
color without leaving any scars or depigmentation. This
is the first report to demonstrate a successful treatment
for improvement of NAC color.
References
1. Yoshimura K, Harii K, Shibuya
F, Aoyama T, Iga T. A new bleaching protocol
for hyperpigmented skin lesions with a high concentration
of all-trans retinoic acid aqueous gel. Aesthetic
Plast Surg 1999; 23: 285-91.
2. Yoshimura K, Harii K, Aoyama T, Iga T. Experience of a
strong bleaching treatment for skin hyperpigmentation in
Orientals. Plast Reconstr Surg 2000; 105: 1097-108.
3. Kligman AM, Willis I. A new formula for depigmenting human
skin. Arch Dermatol 1975; 111: 40-8.
4. Yoshimura K, Tsukamoto K, Okazaki M, et al. Effects of
all-trans retinoic acid on melanogenesis in pigmented skin
equivalents and monolayer culture of melanocytes. J Dermatol
Sci 2001; 27suppl1: 68-75.
5. Yoshimura K, Uchida G, Okazaki M, Kitano Y, Harii K. Differential
expression of heparin-binding EGF-like growth factor (HB-EGF)
mRNA in normal human keratinocytes induced by a variety of
natural and synthetic retinoids. Exp Dermatol, in press.
6. Stoll SW, Elder JT. Retinoid regulation of heparin-binding
EGF-like growth factor gene expression in human keratinocytes
and skin. Exp Dermatol 1998; 7: 391-7.
7. Xiao JH, Feng X, Di W, et al. Identification of heparin-binding
EGF-like growth factor as a target in intercellular regulation
of epidermal basal cell growth by suprabasal retinoic acid
receptors. EMBO J 1999; 18: 1539-48.
8. Chedid M, Hoyle JR, Csaky KG, Rubin JS. Glucocorticoids
inhibit keratinocyte growth factor production in primary
dermal fibroblasts. Endocrinology 1996; 137: 2232-7.
Figure Legends
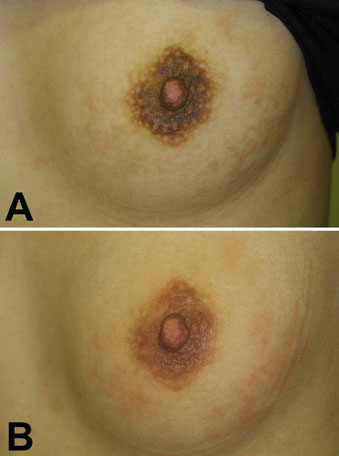
Fig.1. Case 1. A 25-year-old woman
who complained about the color of her NAC and
some pigmentation of the breast mound underwent
the treatment (A: before treatment); 0.2 % tretinoin
gel was used for 4 weeks together with HQ-LA
ointment, followed by application of HQ-LA ointment
alone for 4 weeks (B: after treatment of 8 weeks).
NAC color was improved though the pigmentation
of the breast mound was still observed.
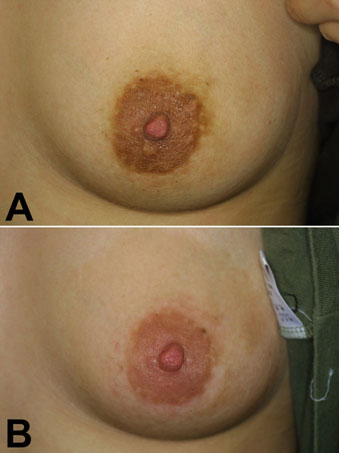
Fig.2. Case 2. A 28-year-old woman underwent the treatment
(A: before treatment); 0.2 % tretinoin gel was used for 4
weeks together with HQ-LA ointment, followed by application
of HQ-LA ointment for 2 weeks and HQ-AA ointments for 4 weeks
(B: after treatment of 10 weeks). NAC color was improved,
but postinflammatory hyperpigmentation was left on the mound
in this case.
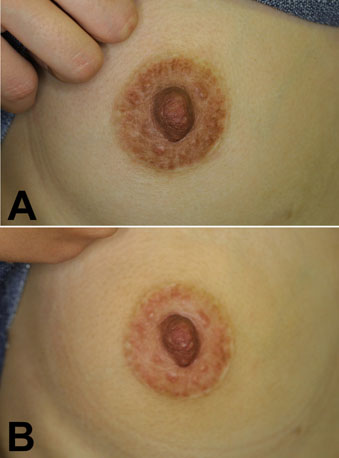
Fig.3. Case 3. A 22-year-old woman
underwent the treatment (A: before treatment).
Because she underwent mastopexy operation before,
she had a linear scar on the areolar margin.
0.2 % tretinoin gel was used for 1 week and 0.4
% tretinoin for 3 weeks, followed by application
of HQ-LA ointment for 6 weeks. (B: after treatment
of 10 weeks). NAC color was improved without
leaving any postinflammatory hyperpigmentation.
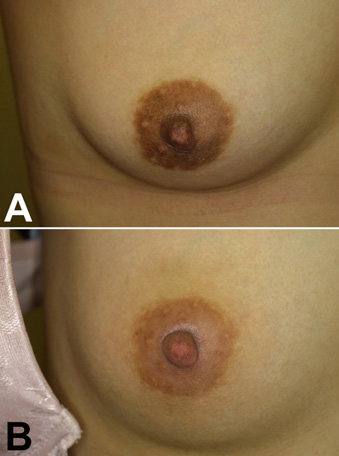
Fig.4. Case 4. A 34-year-old woman
underwent the treatment (A: before treatment).
Bleaching was performed with 0.2 % tretinoin
gel and HQ-LA ointment for 6 weeks, and erythema
disappeared after 6 weeks of healing phase (B:
after treatment of 12 weeks).

Fig. 5. Nipple and areola treated
with laser therapy (the type of laser is unknown)
sometimes demonstrate white scarring. It is almost
impossible to repair the disfiguring appearance.
|